Microbiota Mania
The microbiome is unquestionably essential for good health, but overexaggerated health claims abound
MICROBIOTA
Dr Simon Miller Ph.D.
5/13/20244 min read

The human body is an amazing feat of nature comprising an estimated 30 trillion (30,000,000,000,000) cells. Of course, there is considerable variation among individuals, since this number is only an estimate and was calculated for a textbook male weighing 70 kg.
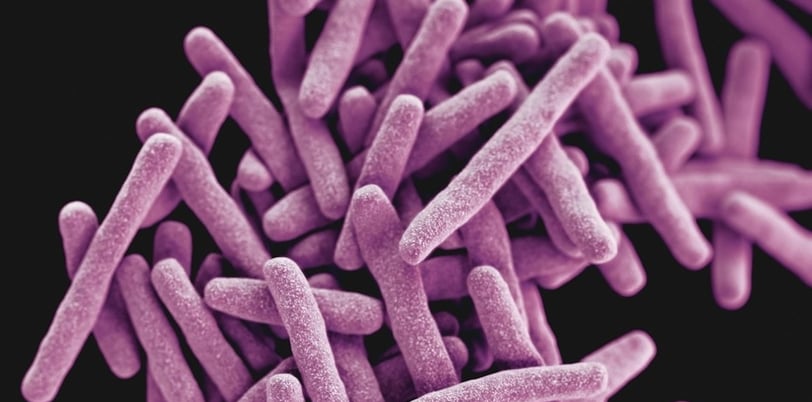
Equally amazing is the fact that microbes typically outnumber human cells with recent estimates putting the number of microbes in and on our bodies at 38–40 trillion. These microbes, collectively known as the microbiota, consist of bacteria, fungi and viruses, and exist on the skin, in the respiratory tract, in the mouth, and, most famously, in the gastrointestinal tract. The actual number of microbes residing in humans, however, can be dramatically different to academic estimates. For example, every time we inhale the number of microorganisms in our lungs will increase and vice versa, bathing will remove millions of microbes from the skin, eating and defecating will dramatically alter the number of organisms in the gastrointestinal tract, and infections and medications (such as antibiotics) will affect bacterial numbers, strain diversity, and microbial DNA. Furthermore, the size and health of an individual can significantly affect the number and variety of microbes.
So what roles do these microbes perform in the body? Well, the human body has an immune system designed to target and kill pathogens, so generally for the body to tolerate microbes there needs to be some mutual benefit or symbiosis. Many strains of “good” bacteria have co-evolved with humans to provide benefits such as complementary genes (transcribed and then translated into proteins) that can metabolise nutrients that human genes/proteins cannot. Moreover, bacteria produce signalling molecules and hormones that play a pivotal role in training the body’s immune system as well as regulating metabolism. Dysfunction of the gut microbiota, known as dysbiosis, has been associated with many diseases such as cancer, heart disease, metabolic disease, dementia, autoimmunity, allergies, inflammatory bowel disease (see What's new in IBD? blog post), and obesity.
Although the gut microbiota is clearly important for metabolic regulation, immunity, and overall health, it is important to note that scientific research data linking the microbiota to diseases are only associations and do not necessarily show causality. Many diseases are multifactorial and the current level of scientific understanding of how to diagnose diseases via microbiome analyses is very limited, let alone therapeutic treatment via probiotic supplementation. Many companies and nutritionists claim to be able to analyse clients’ microbiomes and treat diseases with probiotic supplements; however, extreme caution should be used when considering such services. It is far from trivial to analyse bacterial genomes (microbiomes) from stool samples, because the process is subject to contamination and errors at every stage including sample collection, sample preparation, DNA amplification via PCR, analysis of results, software type and database, and the technician’s handling and experimental protocols. Like everything in life, there is no magic bullet or miracle cure. Moreover, there is the potential for some companies to bypass analyses altogether and just provide arbitrary results to clients. There are scams everywhere, and science, nutrition, and medical health services are no exception.
So what can we do to regulate the health of the gut microbiota? There are two main ways: 1) Prebiotics (dietary nutrients such as fibre and phytochemicals present in whole, unprocessed foods); and 2) Probiotics (live bacteria in some foods such as yogurt as well as in supplemental form). Prebiotics are the best way to nurture and maintain a healthy microbiota, and natural yogurts can be a potential way of obtaining beneficial probiotic bacteria. However, there are caveats to probiotic consumption such as the potential for contamination with harmful bacteria or for so-called "good" bacteria to become bad. Bacterial genomes can be altered via the sharing or passing of DNA from one bacterium to another (known as horizontal gene transfer), or from viral infection of bacterial cells which can switch bacterial genes on or off in a process known as DNA inversion. These genetic modifications can induce antibiotic resistance, virulence, the generation of toxins, inflammation, immune dysfunction, and the onset or exacerbation of disease. For example, DNA inversions have been associated with inflammatory bowel disease. Therefore, even well-intentioned products have the potential for harm, especially since probiotics are not regulated like medications. That being said, naturally fermented products that contain probiotics such as yogurt are generally a safe way to obtain bacterial strains that have been associated with beneficial effects, but supplements are best avoided. This is particularly important for vulnerable individuals with weak immune systems such as the very young, very elderly, and sick people (e.g., cancer patients), who should avoid probiotic supplements and products unless performed under medical guidance.
On a more fundamental level, do we really know what constitutes “good” bacteria? Strong associations have been observed in infant microbiota and infection risk/severity, and multiple studies have shown links among bacterial strains and disease prevention or incidence. However, everyone’s microbiota is unique, and introducing or increasing a particular strain that appears to be beneficial in one individual may not necessarily benefit another individual due to possible incompatibility with the existing microbiota, differences in gene expression, and differences in crosstalk between host immune cells and bacteria.
In summary, do not fall for the marketing hype surrounding gut microbiota analyses and disease treatment with targeted probiotic therapy. Instead, focus on improving the quality of your diet by consuming a wide variety of whole unprocessed foods that are high in fibre and micronutrients, avoid processed foods, avoid dirty or contaminated drinks and foods, and try not to take antibiotics or other medications unnecessarily. Good gut health starts with good nutrition, which is why it is prudent to follow established benchmark diets such as the Mediterranean and DASH diets. The OneLife Diet Meal Plan: Total Nutritional Guide has been carefully constructed to include all the benefits of those established diets but with the added benefit of a greater intake of highly bioavailable protein. This is particularly important for strong immunity and disease prevention when aging as well as healthy weight loss where only fat and not muscle tissue is lost.
Further reading:
OneLife Diet Meal Plan: Total Nutritional Guide. Link
Revised Estimates for the Number of Human and Bacteria Cells in the Body. Link
Inflammation and bacteriophages affect DNA inversion states and functionality of the gut microbiota. Link
Microbiota in health and diseases. Link
Emerging issues in probiotic safety: 2023 perspectives. Link


